Submitted by Jon Anderson, DPT, Therapy Resource
“KO Let’s Go, Let’s Go KO!” This is the rally cry at Keller Oaks in Keller, Texas, and it is a commonly heard anthem when you visit the facility. In a year that has been difficult at best in healthcare, the culture has done nothing but improve at Keller Oaks. When you look deeper to see what is in the air at Keller Oaks, it goes far beyond COVID.
 Kristin Ryther, the therapy program manager at Keller, has been a breath of fresh air in a very trying year at a facility that has been hit hard by COVID on multiple occasions. We asked her to share a bit of her best practices and were blown away by what is developing there.
Kristin Ryther, the therapy program manager at Keller, has been a breath of fresh air in a very trying year at a facility that has been hit hard by COVID on multiple occasions. We asked her to share a bit of her best practices and were blown away by what is developing there.
Starting with onboarding, Keller embraces culture by conducting group interviews and hiring only those people who the team agrees can be grown into great leaders. They agree on all hires and then make sure that the process does not stop there. According to Kristin, “Love is in the details.” She ensures that the new employee is greeted with everything that they need to be successful. She has their log-ins ready, an itinerary for their first day, and a team member assigned to them as a mentor. Kristin provides them with a bit of “swag” and has a ready-made reference form entitled “KO NEED TO KNOW” that includes everything from door codes to restroom locations to documentation tips and PCC locations of interest.
Culture at KO does not stop at onboarding. The team meetings incorporate music and moments of gratitude. Kristin has become a champion of championing others. She works to identify strengths in each of her team members and then assigns responsibilities appropriately. Each member has a strength; slow down and find it! It may be that they have special attention to individual treatments; they may be strong at scheduling, growing programs, or even leading the infection control of the gym. List them out and recognize them.
gratitude. Kristin has become a champion of championing others. She works to identify strengths in each of her team members and then assigns responsibilities appropriately. Each member has a strength; slow down and find it! It may be that they have special attention to individual treatments; they may be strong at scheduling, growing programs, or even leading the infection control of the gym. List them out and recognize them.
Ensure that you are communicating everything to your team. Utilize dry erase boards, address at team meetings, keep up-to-date information in binders. Use all means necessary to ensure that your team members have the communication they need to do their best work! Don’t forget to prioritize individual communication. Get to know your therapists and be transparent as well as approachable. Don’t be afraid to just listen and allow them to be heard.
 Set clear goals and expectations. Kristin sets goals for “2 week sprints.” Some programs are short projects. She assigns a leader and assists with facilitation but allows for teamwork so they meet their goals. She posts the sprints on the communication board, writes about it, takes pictures and then celebrates it. Short-term goals like this make it manageable, and then the challenge is less likely to be pushed off down the road.
Set clear goals and expectations. Kristin sets goals for “2 week sprints.” Some programs are short projects. She assigns a leader and assists with facilitation but allows for teamwork so they meet their goals. She posts the sprints on the communication board, writes about it, takes pictures and then celebrates it. Short-term goals like this make it manageable, and then the challenge is less likely to be pushed off down the road.
Celebrate the wins! Find the team member who loves to do this and assign it to them. Celebrate the day-to-day achievements and find 10 positives for every negative. Make sure the team feels appreciated and celebrated.
That is not to say that there will not be challenges. There will always be hurdles. When that happens, keep your positive vibes on! Start with yourself, and look in the mirror. Stay consistent. Be transparent. Don’t expect others to do something you wouldn’t do yourself. Hold them accountable after you have asked yourself, “Did I educate? Did I communicate? Did I reinforce?” Maintain accountability and expectations, but never be afraid to give each other grace. Most importantly, be yourself! Your team will recognize the authenticity and appreciate the transparency. Let them know it is okay to enjoy your work and have fun while you are doing it!



 This is our first group treatment since October, which is when we went into full lock-down, outbreak mode. It was organized by two of the most compassionate therapists I know, Emily White, PTA, and Wendy Garrison, OTA. The residents had a blast!
This is our first group treatment since October, which is when we went into full lock-down, outbreak mode. It was organized by two of the most compassionate therapists I know, Emily White, PTA, and Wendy Garrison, OTA. The residents had a blast! This is Ron; he was in a catastrophic car accident in 2019, which brought him to us. He received prosthetic training and was set to go home in early November, when he tested positive for COVID. Plans to DC home were postponed, but he made it, and has made it back home to Nebraska.
This is Ron; he was in a catastrophic car accident in 2019, which brought him to us. He received prosthetic training and was set to go home in early November, when he tested positive for COVID. Plans to DC home were postponed, but he made it, and has made it back home to Nebraska. This is Jessica, the Clinical lead and head cheerleader for team Ron. We all cried like babies when he finally went home.
This is Jessica, the Clinical lead and head cheerleader for team Ron. We all cried like babies when he finally went home. As a compromised patient, Glenna should not have survived, according to all our knowledge of the virus, but she did. What a happy day it was to move her off of the COVID wing back to her own room.
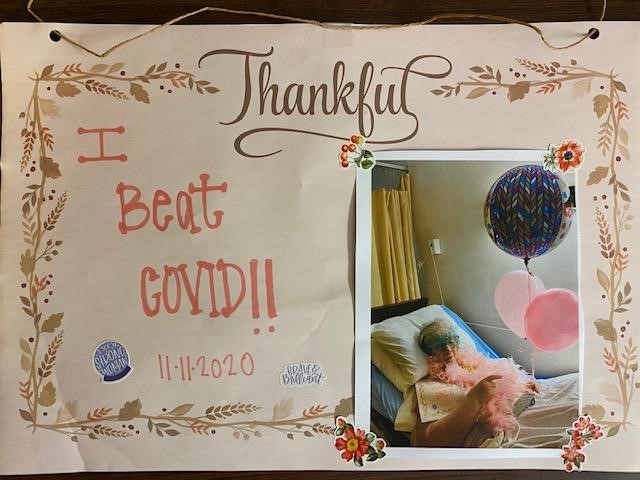
As a compromised patient, Glenna should not have survived, according to all our knowledge of the virus, but she did. What a happy day it was to move her off of the COVID wing back to her own room. This was our very first survivor. She didn’t even know she was sick and was happily confused about all the fuss we were making over her. We are all truly thankful for the opportunity to celebrate with her. (photo of thankful I beat COVID)
This was our very first survivor. She didn’t even know she was sick and was happily confused about all the fuss we were making over her. We are all truly thankful for the opportunity to celebrate with her. (photo of thankful I beat COVID)
 Denise Del Cano, COTA, ADOR, has dedicated her career in The Hills Post Acute. An alumnus of Santa Ana College, she earned her associate’s degree in Occupational Therapy Assistant 12 years ago and has been with the facility since then. She was promoted to Assistant Director of Rehab last year and completed the DORITO program this year. Denise did her internship here at The Hills. She was supervised by Vonda Gaier, COTA, who then became her colleague. She is a Filipino American born in Los Angeles, California, the eldest of five and a loving mother to her 16-year-old daughter, Elizabeth. Interestingly, Denise was introduced to the field of therapy when her daughter received therapy for several years. Denise saw the importance and relevance of Occupational Therapy and has been an advocate ever since.
Denise Del Cano, COTA, ADOR, has dedicated her career in The Hills Post Acute. An alumnus of Santa Ana College, she earned her associate’s degree in Occupational Therapy Assistant 12 years ago and has been with the facility since then. She was promoted to Assistant Director of Rehab last year and completed the DORITO program this year. Denise did her internship here at The Hills. She was supervised by Vonda Gaier, COTA, who then became her colleague. She is a Filipino American born in Los Angeles, California, the eldest of five and a loving mother to her 16-year-old daughter, Elizabeth. Interestingly, Denise was introduced to the field of therapy when her daughter received therapy for several years. Denise saw the importance and relevance of Occupational Therapy and has been an advocate ever since. As we persevere through the pandemic, I am often reminded how fortunate I am to have such wonderful teammates. I continue to be the proudest team leader.
As we persevere through the pandemic, I am often reminded how fortunate I am to have such wonderful teammates. I continue to be the proudest team leader.



 By Milena Milenkovic, OT/DOR, Park View Post Acute, Santa Rosa, CA
By Milena Milenkovic, OT/DOR, Park View Post Acute, Santa Rosa, CA