By Nicole King MA, CCC-SLP, Julia Temple Health Care Center, Englewood, CO
Use meal times to your advantage! Not only can you check in on your swallowing patients, but it is a great time to address following directions, sequencing, and attention during simple functional tasks — such as adding cream and sugar to their coffee, hand hygiene, cutting up their food, etc.
It is also a great time to address communication and social interactions. The facility is their home. Tasks that might not be functional for your skilled population are functional and meaningful in LTC and memory care neighborhoods — for example, deciding which snack they want, finding their room, participating in activities, and deciding when and where they will eat.
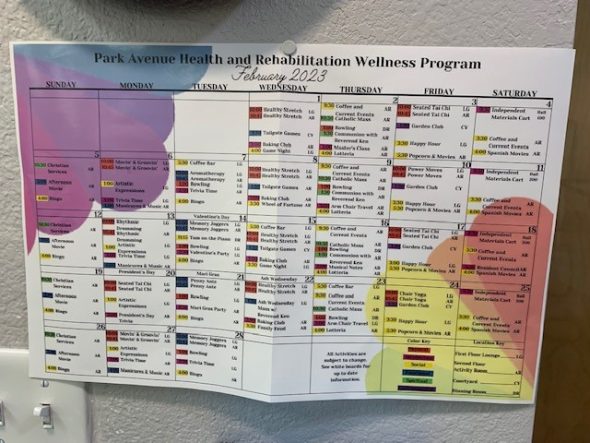
Partner up with Activities or the Chaplain. They can provide the task, but you can provide the skilled eye, environmental modifications, and dynamic cueing that allows the residents to participate in a meaningful and engaged way. Maybe your restless patient needs to be able to come and go from the area, or certain residents shouldn’t sit near each other. It could be the resident needs parallel involvement that allows them to participate but with less environmental stimuli and/or distractions.
Don’t be afraid to “hang out” in the memory care neighborhood. Using a naturalistic approach allows you to see patterns in behavior, identify triggers of agitation, find other patients to evaluate, and get to know the staff better. I also try to do my documentation there because it provides me with more time to observe and engage.
Take credit for what you are doing! Don’t assume that the intervention or strategy is obvious to everyone. Sometimes the smallest change can make all the difference. At JT, we had a patient who played with her food during meals and it upset nearby residents. After assessing her response to her environment over a few meals and analyzing how she engaged with her surroundings and staff, it hit me. She only played with her food on the days her appetite was low. It was her way of letting us know she was full.
Think outside the box and step out of your comfort zone! Let go of the idea that your therapy should look a certain way. Language and communication opportunities are everywhere. Remember it isn’t always about restoring lost skills/function, but changing the environment or how we interact with them, or creating opportunities for them to succeed based on the skills they still have.
Documentation. We all know documentation is important, but with LTC therapy and skilled maintenance, it is crucial. To an outsider, it might look like you just sat next to a patient during an activity. But what you actually did was “facilitated optimal patient participation during preferred leisure task by incorporating dynamic cueing hierarchy, environmental modifications, errorless learning techniques, and spared skills.” Always document the functions or presentations that you assessed in order to know what to do, and exactly how what you saw guided the interventions you selected. The skill lies in the assessment you performed, and how you acted on that assessment.
Goals. The questions I get asked most frequently are related to setting goals. Here are a few of my favorites:
- Patient will demonstrate ability to use verbal and nonverbal communication to make decisions related to preferences during care tasks and daily routine with MOD A to facilitate highest level of independence on nursing unit
- Patient will maintain ability to complete 3-4 conversational exchanges related to direct and observable topics using multisensory stimuli in order to reduce risk of social isolation and decrease in meaningful interactions
- Patient will maintain current level of cognitive communication function to actively participate (following along with handout, switching between tasks, singing along, etc.) in weekly worship service with MIN-MOD A in order to preserve quality of life and highest level of independence with leisure activities of choice
- And finally, remember that being able to support ongoing therapy for maintaining function requires evidence that only you can do what needs to be done. Once the patient’s function looks consistent, or what you need to do changes very little from session to session then it’s time to phase yourself out and hand over those activities to others.