
By Brian del Poso, Associate Compliance Partner
With just about three-fourths of the year completed, it’s a good time to provide an update on where we stand compliance-wise and what’s on the horizon for the rest of the year. Therapy documentation and technical accuracy has come a long way, so kudos to all of you. There are still a few areas, however, that we can pay closer attention to. These items will sound familiar as they have been identified in years past and have improved, but we definitely still need to consistently get better at:
- Physical agent modalities documentation
- Co-tx documentation
- Personalized clinical assessment in Progress Reports
- Documentation and justification for billing patient education, especially when residents are difficult and/or refusing treatment
Again, there has been improvement in these areas, but there’s definitely a high ceiling for growth. I encourage you all to seek further education and training in these documentation areas. The easy way out would be to look at some of these things and just say, “Well, we just won’t do co-tx anymore,” or “We don’t use physical agent modalities often, so…,” but the easy way out isn’t who we are. Let’s invest in each other and in the spirit of our core value of PASSION FOR LEARNING, and utilize the therapy resources, POSTettes, and compliance partners we have at our disposal to move ourselves forward.
Part A MSCAs were on a bit of a hiatus as the IRO summer season began, but they are starting up again as we speak. With that said, here’s a YTD look at some of our top-performing facilities from the MSCAs. Congrats and keep it up!
| 2018 MSCA Overall Scores | 2018 MSCA Therapy Dept. Scores | |||
| Facility | Top 5 | Facility | Top 5 | |
| Timberwood (Keystone) | 99.27% | The Grove (Signum) | 100.00% | |
| Panorama Gardens (Signum) | 99.11% | Golden Acres (Keystone) | 99.53% | |
| Brookside (Signum) | 99.04% | Northbrook (Signum) | 99.53% | |
| Claremont (Signum) | 98.45% | Atlantic (Signum) | 99.43% | |
| Sea Cliff (Signum) | 98.39% | Brookside (Signum) | 99.40% | |
If you’d like to know where you rank within your company, please reach out to your local compliance partner, and we will get that information out to you.
Coming up in Q4, we’ll be wrapping up any leftover MSCAs, and similar to recent years, we will also be starting up Part B MSCAs. As a reminder, not all facilities will receive a Part B audit this year. Facilities chosen for Part B audits will be dependent on the size of your Part B program. Essentially, if your YTD Part B revenue hits a certain threshold, you’ll be in the pool for a Part B audit. We’re currently working on the threshold to see how much revenue makes sense for a cutoff point, so more to come from your local compliance partners.
Lastly, I’m sure you all have heard or seen the emails about our Independent Review Organization (IRO) audits. We’re not out of the woods yet and still have the remote portion coming up, but we wanted to give a shoutout to this year’s on-site facilities (Legend Oaks Kyle, Golden Acres, Rehab Center of Des Moines, Grand Oak, Redmond, HCR CO Springs, Heritage Park, Brookfield) for doing such an awesome job in our very last CIA and IRO year!




 By Lori O’Hara, MA, CCC-SLP – Therapy Resource, ADR/Appeals/Clinical Review
By Lori O’Hara, MA, CCC-SLP – Therapy Resource, ADR/Appeals/Clinical Review
 Congratulations to our newest SPARC Award Winner, Hannah Ruth Downing, SLP Student at Sacramento State University, Grad Date 5/19/2019
Congratulations to our newest SPARC Award Winner, Hannah Ruth Downing, SLP Student at Sacramento State University, Grad Date 5/19/2019
 Physical therapy can treat OAB through utilization of Medtronic NURO system. How does this therapy work? Medtronic Bladder Control Therapy delivered by Medtronic NURO system restores bladder function by stimulating the tibial nerve through an acupuncture-like needle placed near the ankle.
Physical therapy can treat OAB through utilization of Medtronic NURO system. How does this therapy work? Medtronic Bladder Control Therapy delivered by Medtronic NURO system restores bladder function by stimulating the tibial nerve through an acupuncture-like needle placed near the ankle.


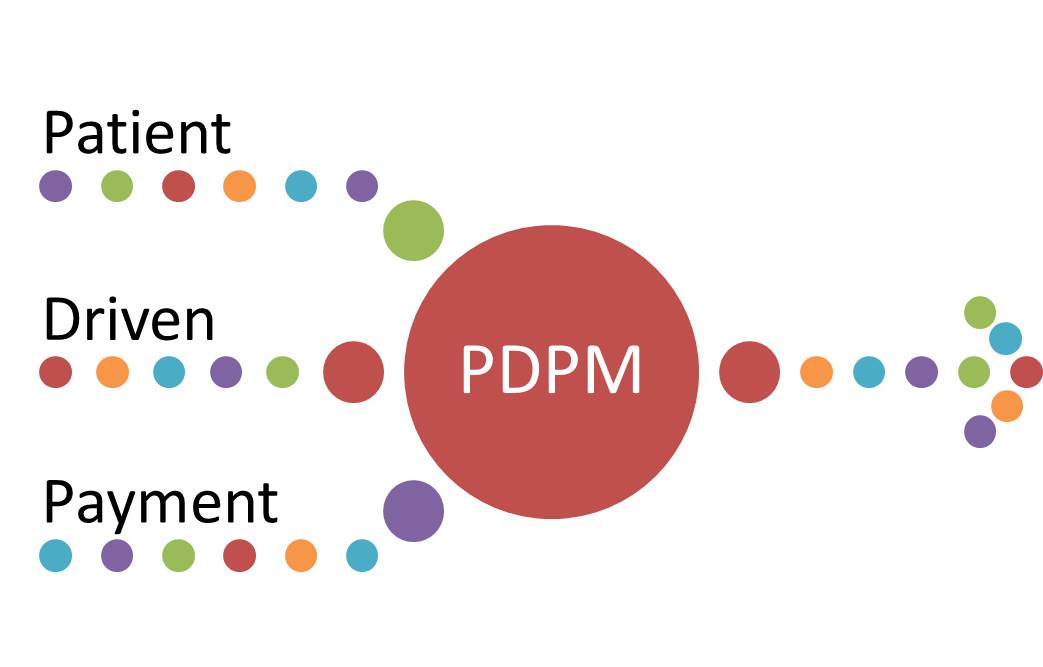
 The proposed rule Fiscal Year 2019 has been considered by many to be the most anticipated rule proposal since the introduction of the Medicare Prospective Payment System in 1998. The NPRM was released to the public on Friday, April 27, 2018, and introduced us to a new payment model entitled, the Patient Driven Payment Model (PDPM), which is suggested in the rule to become effective in October 2019.
The proposed rule Fiscal Year 2019 has been considered by many to be the most anticipated rule proposal since the introduction of the Medicare Prospective Payment System in 1998. The NPRM was released to the public on Friday, April 27, 2018, and introduced us to a new payment model entitled, the Patient Driven Payment Model (PDPM), which is suggested in the rule to become effective in October 2019.